Research on childhood cancer has been slow to progress when compared to adult cancer. While childhood cancer is less common than cancer in adults, it’s the leading cause of disease-related death in Canadian children. Meanwhile three in five childhood cancer survivors go on to experience lifelong side effects.
Dr. Alexandra Zorzi, a researcher at Lawson Health Research Institute and paediatric hematologist/oncologist at Children’s Hospital at London Health Sciences Centre (LHSC), is working to improve patient outcomes by driving childhood cancer research forward.
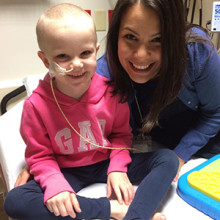
Above: Dr. Alexandra Zorzi (right) with six-year-old patient, Hayden (left)
Personalized medicine for childhood cancer
In one project funded through Children's Health Foundation, Dr. Zorzi has partnered with fellow Lawson scientist, Dr. Richard Kim, to study pharmacogenomics for childhood cancer. Dr. Kim is a world-renowned expert on pharmacogenomics, or ‘personalized medicine,’ which is the study of a patient’s unique DNA to predict how he or she will respond to a particular medication.
For some patients, genetic changes alter the way a drug is metabolized in their body which can disrupt its effects and heighten its toxicity. Pharmacogenomics analyzes patient blood samples through a process called genotyping to ensure patients are prescribed the right dose of the right medication at the right time.
Drs. Zorzi and Kim are currently examining childhood cancer patients’ genetic makeup and comparing it to treatment outcomes. The goal is to eventually use this knowledge to predict how patients will metabolize a particular chemotherapy, as well as other drugs commonly used for childhood cancer patients like anti-nausea medications. To date, they’ve enrolled an impressive 100 research participants in the study.
“We’re looking to not only determine if the dose will be effective in treating the cancer, but also to predict its toxicity,” says Dr. Zorzi. “We know childhood cancer survivors have significant, long-term effects from therapy. It’s our goal to not only cure childhood cancer but ensure survivors have as minimal impact from treatment as possible.”
Drs. Zorzi and Kim have already opened a sub-study of this personalized medicine project to look at a specific chemotherapy drug called 6-Mercaptopurine (6MP), which is used in the treatment of acute lymphoblastic leukemia (ALL). There’s a known enzyme involved in the metabolism of this drug and genetic changes could influence the way it’s dosed. The research team has now discovered new additional proteins involved in drug transport that could be just as important in the metabolism of 6MP. They’ve enrolled 30 research participants in a study that will examine the role of these proteins more closely.
“We’re incredibly excited about the potential of pharmacogenomics for childhood cancer,” says Dr. Zorzi. “If successful locally, we hope to eventually expand on a national level.”
Targeting the tumour
In another project, Dr. Zorzi has joined a national initiative called PROFYLE. PROFYLE, which stands for ‘PRecision Oncology For Young peopLE,’ focuses on those patients with difficult to treat and poor prognosis tumours.
“There’s a group of childhood cancer patients whose outcomes and prognosis have not changed significantly in the past 30 years. This includes patients with solid tumours like sarcomas, brain tumours and cancers that return after treatment,” says Dr. Zorzi. “These patients continue to have an unacceptable cure rate.”
The project, led by the Terry Fox Research Institute (TFRI), examines the unique molecular profile or ‘fingerprint’ of a tumour to identify any gene mutations that might match a target for a particular drug. Also known as ‘targeted therapy,’ this includes matching patients with pre-existing drugs that have not traditionally been used against the cancer in question.
“For example there may be a drug therapy that isn't traditionally used for that particular cancer but that makes sense given the genomic makeup,” explains Dr. Zorzi. “With PROFYLE, we are able to identify these genomic changes to hopefully offer a therapy we would have never considered based on pathology alone.”
With $16.4 million in funding the goal of PROFYLE is to provide new hope to all Canadian children with relapse cancer. The project, born from pilot projects at The Hospital for Sick Children (SickKids) in Toronto, British Columbia Children’s Hospital and Montreal Children’s Hospital, brings together research centres, children’s hospitals, cancer charities and foundations from across the country. In addition to matching patients with targeted therapy, the project aims to build our understanding of whether some children are predisposed genetically to develop cancers.
Eligible research participants have their tumour biopsied and sent to one of three sequencing centres in Canada, located in Toronto, Montreal and Vancouver. Once a tumour is sequenced, the patient’s oncologist and the research team meet virtually to discuss relevant findings. They attempt to match the patient with a drug that targets the tumour’s ‘fingerprint’ through open clinical trials, marketed agents or novel therapeutics.
A similar method is being studied with cancer in adults. A national study called the ‘CAnadian Profiling and Targeted agent Utilization tRial (CAPTUR)’ matches adult cancer patients with commercially available drugs that target their tumour’s ‘fingerprint.’ Lawson is one site for this study with Dr. Stephen Welch as a local lead. Dr. Zorzi is working to open up a sub-study study called ‘CAPTUR paediatrics’ that would help match PROFYLE patients to the drugs they need.
“Access to medications in paediatrics is difficult. Sometimes matching the tumour with a drug is just the first step of a huge hurdle,” says Dr. Zorzi. “In the case of PROFYLE, the use of medications is considered ‘off label.’ They might not currently be approved for use in children or for the cancer in question. The medication may not even be licensed in Canada. CAPTUR paediatrics would work to provide easier access to such medications.”
One family’s journey
For the Morton’s, a family from Strathroy, Ontario, a childhood cancer diagnosis was the start of a long and difficult journey. Advancing research is a cause close to their hearts.
Robby Morton was just shy of 16 when he was diagnosed with osteosarcoma - a type of bone cancer. He was diagnosed in 2016 on a visit to the emergency department when an x-ray revealed the cancer in his leg. Robby’s diagnosis was followed by months of treatment and surgeries, including a leg amputation that involved four surgeries in six days.
“Robby signed up for every research opportunity that was presented to him,” says Wendy Morton, Robby’s mother. “While many of the projects were early and wouldn’t improve the course of his treatment, he knew it could help future childhood cancer patients and that was important to him.”

Above: The Morton family (from left) - Corbin, Julie, Robby and Wendy
While Robby’s surgeries went well, Robby’s chemotherapy treatments did not. “The chemotherapy was not very effective for his tumour but there were no other viable options to pursue,” explains Wendy.
In a follow-up appointment after his initial chemotherapy treatments, Robby’s care team discovered that the cancer had spread to spots in his lungs. These spots were removed and more chemotherapy followed.
While Robby participated in research projects like PROFYLE, no eligible clinical trials in Canada were found for his cancer. When looking at other clinical trials, the drugs that might have benefitted Robby were not accessible.
The cancer continued to spread and Robby passed away in August 2018.
“Children with cancer don’t need miracles; they need research. It’s incredibly sad that it’s been 30 years without improvements in treatment for children whose cancers have spread or returned,” says Wendy. “As initiatives like PROFYLE continue to develop and more people contribute to the bank of knowledge, I hope things will improve. But we need to ensure the drugs are available, which is why Dr. Zorzi’s work in bringing clinical trials to London is so important.”
Dr. Zorzi has worked to open Lawson’s first early phase (phase I and phase II) clinical trials for recurrent or relapsed solid tumours, and is currently working to open other industry trials looking at immunotherapy. “Unfortunately, we have the patient volumes to open these trials,” Dr. Zorzi says. “They provide new opportunities for local patients without them needing to travel to other sites like Toronto.”
Moving forward, Dr. Zorzi hopes to bring an increasing number of clinical trials to Lawson and improve access to new childhood cancer therapies in Canada.
Drs. Kim and Zorzi's research on pharmacogenomics for childhood cancer is funded through Children's Health Foundation. Dr. Zorzi’s research has also been supported with funding from Childcan, a Lawson Internal Research Fund (IRF) grant and a grant from LHSC’s London Regional Cancer Program.


