Personalized medicine is the analysis of a patient’s DNA to predict how they will respond to medications. Led by Dr. Richard Kim, scientist at Lawson Health Research Institute (Lawson) and clinical pharmacologist at London Health Sciences Centre (LHSC), researchers at Lawson have received $4.4 million to study an expanded personalized medicine program at LHSC. One third of the funding comes from the provincial government’s Ontario Research Fund (ORF) while the remainder is contributions from Thermo Fisher Scientific and donor funding through London Health Sciences Foundation.
Personalized medicine uses pharmacogenomics - the study of genetic changes that alter the way a person responds to individual drugs. The new funding will enable researchers to follow patient outcomes and assess the cost-effectiveness of LHSC’s personalized medicine program, providing evidence on the relationship between the cost of the program and how patient care is improved.
LHSC’s personalized medicine program involves full integration of research into patient care. Research questions are informed by the therapeutic challenges seen in hospital. As research discoveries are made, they are then applied back to patient care. LHSC was the first in Canada to implement personalized medicine as a clinical strategy. The practice began in 2008 through Dr. Kim’s research on warfarin – a blood thinner prescribed to treat blood clots.
For every drug there are patients whose bodies cannot metabolize or process it properly. The drug may not work and can even be toxic. When a medication is toxic, patients can experience an adverse drug reaction where they respond poorly. Adverse drug reactions are the fourth leading cause of death among hospitalized patients and cost the Canadian health care system over $5 billion a year.
“For every medication there are patients who should be prescribed lower or higher than the recommended standard dose and patients who should be prescribed an entirely different medication,” explains Dr. Kim. “Personalized medicine studies a patient’s unique DNA to ensure he or she is prescribed the right dose of the right medication at the right time.”
The team’s research has grown since 2008 and this funding will help provide testing for a number of other drugs. For example, they can now offer testing for cancer patients prescribed 5-fluorouracil. This particular chemotherapy is associated with high toxicity but is very important in treating bowel, stomach and head and neck cancers.
Oncologists at LHSC’s London Regional Cancer Program (LRCP) can now refer patients for testing before their first dose of 5-fluorouracil. The Personalized Medicine team meets with the patient at one of their twice-weekly clinics, obtains consent and takes a blood sample. The team then performs a test called genotyping to study the patient’s genetics and predict their response to 5-fluorouracil. A full report is generated and sent back to the referring oncologist.
If it’s predicted a patient will respond poorly to the drug, the team follows clinical guidelines to make recommendations to the patient and the referring physician. This often involves changing the dose or finding an alternative therapy.
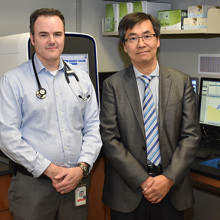
Dr. John Lenehan (left), oncologist at London Health Sciences Centre’s London Regional Cancer Program, and Dr. Richard Kim. Dr. Lenehan’s patients benefit from the Personalized Medicine program and the testing of 5-fluorouracil.
“We want to take drugs that are shown to be beneficial and make them even safer and more effective by tailoring them to the individual,” continues Dr. Kim. “By showing that medications are not ‘one size fits all,’ we can reduce toxicity, enhance outcomes and lower health care costs.”
The team will study the outcomes of any patients referred to the program, including hospital stays, emergency department visits and physician visits. These patients will be compared to others in the province using provincial health care data from the Institute for Clinical Evaluative Sciences (ICES). The team hopes to demonstrate the cost-effectiveness of implementing personalized medicine in a large acute-care hospital in Ontario.
“We will examine patients’ healthcare utilization to prove how effective our program can be,” adds Dr. Kim. “Through the development of secure and scalable technologies as well as a personalized model of patient care, we hope to demonstrate that our model of personalized medicine can be adopted by other health care providers across the province as an innovative and cost-effective way to enhance the health of Ontarians.”
In addition to the ORF funding, Dr. Kim acknowledges the importance of donors to this research project. Thermo Fisher Scientific, a leader in pharmacogenomics technology, provided the team with cutting-edge technology that helps them to test more patients for more genetic variations at the same time. This further enables the team’s work.
Through the London Health Sciences Foundation, the project has seen significant contributions, including $2.24 million from LHSC’s Auxiliary and $300,000 from 3M Canada.
“This is a prime example of donors further enabling our work,” says Dr. Kim. “Through research, donor dollars can make a lasting impact to patient care.”
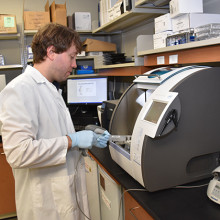
Cameron Ross (above), a research assistant in Dr. Kim’s lab, using the lab’s genotyping equipment.


