Recharting the course of Alzheimer’s disease
“The importance of this research on the community cannot be overstated,” shares Sarah Best, Research Manager, about the work in Alzheimer’s disease happening inside the walls of St. Joseph’s Health Care London right now – projects sustained by donor funding. “Our population is aging, and the biggest risk factor for most neurodegeneration, such as Alzheimer’s disease, is age.”
There are several research groups at St. Joseph’s focusing on early detection, new treatments and recommendations for people going through the challenging journey of Alzheimer’s disease, including the Cognitive Clinical Trials Group led by Dr. Michael Borrie and the Brain and Gait Lab led by Dr. Manuel Montero-Odasso. Catching the disease early can extend someone’s independence as they grow older.
“Early detection not only impacts quality of life for the individuals experiencing this horrible disease, but also their family and caregivers as their lives change, too,” shares Sarah. “If we could delay the onset of dementia by five years, it would reduce the prevalence by 57 per cent. That’s a huge number.”
We all experience forgetfulness from time to time. But for people living with Alzheimer’s disease or dementia, the cognitive challenges are intense and constant. They might struggle to remember the day of the week, where they live or how to perform daily tasks. Their emotions shift from fear to sadness to dread. And everyone’s experience with the disease is different.
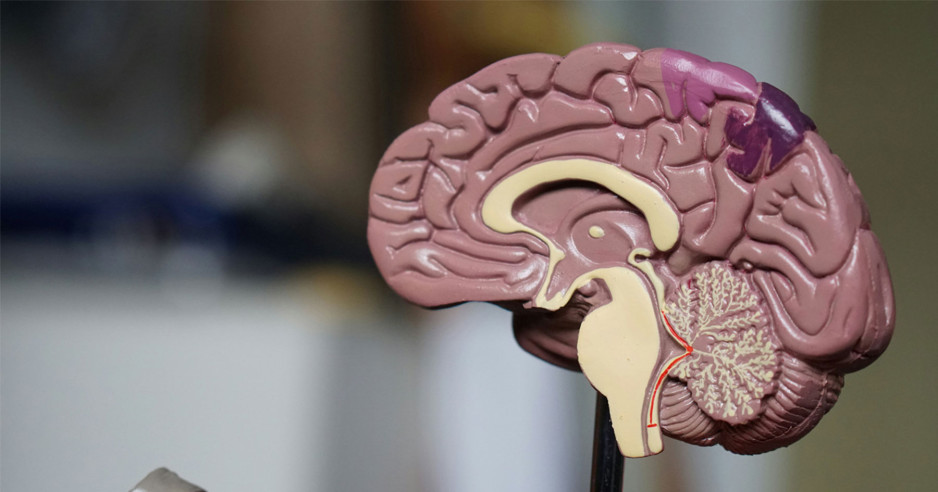
Alzheimer's disease is the most common cause of dementia, accounting for nearly 80 per cent of dementia cases. Researchers continue to investigate the origins of the disease, and it may be linked to an abnormal buildup of proteins called amyloid plaques and tau tangles in the brain that affect cell function.
But what if there was a way to remove those protein buildups and slow someone’s cognitive and functional decline?
In 2023 and 2024, two disease modifying treatments to slow Alzheimer’s disease in its early stages were approved in the United States. These novel medications, that might be able to target and destroy the proteins that cause Alzheimer’s disease, are currently under review by Health Canada.
St. Joseph’s researchers contributed to this global breakthrough through years of studies and clinical trials. Their pioneering work would not be possible without the generosity of individuals and organizations across the region who know the pain of dementia firsthand and value the promise of clinical research. Over the years, donors including the Alzheimer’s Society have helped to support many projects at St. Joseph’s aimed at uncovering new approaches to care. Today, donor support continues to play a key role in funding the future of research in this field.
With Health Canada’s approval of the disease-modifying medications on the horizon, St. Joseph’s researchers are now launching a “homegrown” biomarker study of local patients. Once the new medications are available, it’s vital that care providers can quickly and accurately diagnosis people at risk of developing dementia due to underlying Alzheimer’s disease. If their biomarkers are positive, they may be eligible for this treatment – the sooner, the better.
This new study – named BioMIND – is helping to identify and address barriers to accessing the new medications and improve outcomes for people currently on waitlists for care. The team at St. Joseph’s plans to enroll 100 participants who will be offered different tests for biomarker analysis including lumbar punctures, MRI scans and blood draws that, over time, could indicate if their disease is progressing and may respond to treatment. The research team is aiming to determine the best way to triage people for a potentially life-changing prescription.
“Just having knowledge is power,” says Sarah. “People haven’t been able to have that clarity of diagnosis yet. These biomarkers will really change how people are diagnosed and help them plan for their future. We’re able to work on big projects, but we also get to think about our own community and address issues right here through research.”
The research teams are excited about the possibility of a new future of care for our aging population – and grateful to donors for funding their work. “We work in a really hard area. It’s hard for people living with these diseases,” Sarah says. “But now I feel like we have a lot of hope.”